Bridging the Digital Gap: The NHS 10-Year Plan and the Shift Towards Digital Health
- Dr Catia Nicodemo

- Aug 8
- 6 min read
Updated: Aug 12
Introduction
In an era where technology has reshaped nearly every aspect of our lives—from how we bank to how we learn—healthcare has often been slower to adapt. Yet, the NHS Long Term Plan, published in July 2025, set out an ambitious vision to change that. Over the next decade, the NHS aims to harness digital innovation to create a more efficient, patient-centered health system. One of the most significant shifts is the move towards digital health apps and remote care, designed to give patients greater control over their health while easing the burden on traditional services.
However, this digital transformation doesn’t come without challenges. While many embrace the convenience of health apps and online consultations, others risk being left behind. The digital divide—the gap between those who can easily access and use technology and those who cannot—remains a pressing issue. Older adults, people on low incomes, and those with limited digital skills may struggle to navigate this new landscape, potentially widening health inequalities rather than closing them.
In this blog, we’ll explore how the NHS plans to integrate digital health solutions over the next decade, the benefits these changes could bring, and the steps needed to ensure that no one is excluded from the future of healthcare.
The NHS 10-Year Plan: A Digital Revolution in Healthcare
The NHS Long Term Plan is more than just a policy document—it’s a roadmap for transforming healthcare in England. At its core is a commitment to prevention over cure, personalized care, and digital innovation. The goal is to create a health service that is not only more efficient but also more responsive to the needs of patients.
The Rise of the NHS App and Digital Services
One of the most visible changes has been the expansion of the NHS App, which acts as a digital front door to healthcare services. Through the app, patients can book GP appointments, order repeat prescriptions, and access their medical records—all from their smartphone. The plan is to go even further, integrating AI-powered symptom checkers and personalized health advice to help people manage their conditions more effectively.
Remote Monitoring and Virtual Wards
For those with long-term conditions like diabetes or heart disease, regular hospital visits can be time-consuming and stressful. The NHS is addressing this by rolling out remote monitoring tools that allow patients to track their health at home. Wearable devices can send real-time data to healthcare teams, alerting them to any concerning changes. Some hospitals have even introduced "virtual wards", where patients receive hospital-level care in their own homes, reducing the need for lengthy admissions.
AI and Data-Driven Healthcare
Artificial intelligence is playing an increasingly important role in the NHS. Predictive analytics can help identify patients at high risk of complications, enabling early intervention. Meanwhile, automated triage systems are being tested to help GPs prioritize cases more efficiently, ensuring that those who need urgent care receive it faster.
Tackling Health Inequalities
While these innovations promise to improve care for many, the NHS is acutely aware that not everyone is ready—or able—to embrace digital health. The plan includes measures to support those at risk of being left behind, from digital literacy training to ensuring alternative options remain available for those who need them.
The Promise of Digital Health Apps
Digital health apps have the potential to revolutionize how we manage our well-being. They put power in the hands of patients, allowing them to take a more active role in their care. Apps like MyCOPD help people with chronic lung disease track their symptoms and adjust their treatment, while Oviva provides personalized nutrition coaching for those with diabetes. Meanwhile, AI-driven platforms like Babylon Health offer instant access to medical advice, reducing the need for unnecessary GP visits.
The success of the NHS App demonstrates the appetite for digital health solutions. Since its launch, it has been downloaded by millions, with many users praising its convenience. Research suggests that it has already helped reduce the number of phone calls to GP surgeries for simple tasks like prescription renewals, freeing up staff to focus on more complex cases.
Yet, despite these benefits, adoption is not universal. For some, the shift to digital feels daunting, or even exclusionary.
The Digital Divide: Who’s Being Left Behind?
While digital health tools offer enormous potential, their benefits are not evenly distributed. Several key barriers prevent universal access:
Limited Digital Literacy
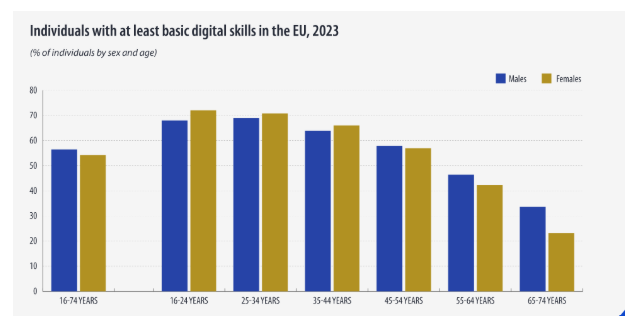
A significant portion of the UK population—particularly older adults—struggles with basic digital skills. According to a 2023 report by Lloyds Bank, around 5 million people lack the confidence to use online services effectively. For these individuals, navigating health apps or virtual consultations can feel overwhelming, leaving them reliant on traditional, often overstretched, services.
Access to Technology
Not everyone owns a smartphone or has reliable internet access. In low-income households, the cost of devices and data plans can be prohibitive. Even when technology is available, poor connectivity in rural areas can make digital health services frustrating or unusable.
Preference for Face-to-Face Care
For many, healthcare is deeply personal. Some patients, particularly older generations, value the reassurance of speaking to a doctor in person. While digital options can improve efficiency, they must not come at the expense of human connection.
Bridging the Gap: Ensuring Inclusive Digital Healthcare
The NHS’s digital transformation cannot succeed unless it works for everyone. Here’s how we can make that happen:
1. Invest in Digital Literacy Programs
Community-based training can help people build the skills they need to use health apps confidently. Libraries, GP surgeries, and local charities could play a key role in delivering this support.
2. Provide Alternative Access Routes
While digital services should be encouraged, phone and in-person options must remain available for those who need them.
3. Address Affordability Barriers
Schemes that provide discounted or free devices to low-income households could help close the access gap.
4. Design with Accessibility in Mind
Health apps should be intuitive and user-friendly, with features like voice commands and large text options for those with visual or cognitive impairments.
Conclusion: A Digital Future, But Not at the Expense of Inclusion
The NHS’s 10-year plan represents an exciting step forward, harnessing technology to create a more responsive and sustainable health system. However, the success of this transformation depends on ensuring that no one is left behind. By addressing the digital divide head-on—through education, accessibility, and inclusive design—we can build a healthcare system that truly works for everyone.
The future of health is digital, but it must also be fair, flexible, and human-centered. Only then can we ensure that the benefits of innovation reach every corner of society.
The Road Ahead: Sustaining Momentum in Digital Health
As we look towards the next decade, the NHS faces both opportunities and challenges in realizing its digital ambitions. The rapid pace of technological advancement means that new tools and platforms will continue to emerge, offering even greater potential to transform patient care. However, sustaining this momentum requires ongoing investment, collaboration, and a commitment to inclusivity.
Strengthening Digital Infrastructure
For digital health to thrive, the underlying infrastructure must be robust. This means not only improving broadband connectivity across the country but also ensuring that NHS systems are interoperable, allowing seamless data sharing between different healthcare providers. Cybersecurity will also be a critical concern, as the increasing reliance on digital platforms makes the NHS a potential target for cyberattacks.
Engaging Communities in the Digital Transition
True digital inclusion requires more than just providing technology—it demands active engagement with communities to understand their needs and concerns. Public awareness campaigns can help demystify digital health tools, while partnerships with local organizations can ensure that support reaches those who need it most.
Balancing Innovation with Equity
As the NHS embraces cutting-edge technologies like AI and machine learning, it must also guard against exacerbating existing inequalities. Algorithms trained on biased data could inadvertently disadvantage certain groups, while over-reliance on digital solutions might alienate those who prefer traditional care. Striking the right balance will be key to building a health system that is both innovative and equitable.
Measuring Success Beyond Numbers
While metrics like app downloads and virtual consultations serve as valuable indicators of progress, the true measure of success lies in improved health outcomes and patient satisfaction. Regular feedback from users—especially those from marginalized groups—will be essential in refining digital services to better meet their needs.
Final Thoughts: A Collective Responsibility
The NHS’s digital transformation is not just a task for policymakers or technologists—it’s a collective responsibility that involves healthcare professionals, community leaders, and patients themselves. By working together, we can ensure that the shift to digital health enhances rather than undermines the principles of universality and accessibility that define the NHS.
The journey ahead will undoubtedly present challenges, but the potential rewards—a healthier population, a more sustainable health system, and a society where everyone can benefit from technological progress—are well worth the effort. As we navigate this digital frontier, let us remain guided by the core values of compassion, equity, and inclusion that have always been at the heart of the NHS.
In the end, the success of the NHS’s 10-year plan won’t be measured by the sophistication of its technology, but by its ability to deliver better care for all, regardless of age, income, or digital literacy. That is the true promise of a digitally empowered future.